The nutrition scientist Ancel Keys shaped our understanding of fat and heart health with the Seven Countries Study – but his contemporary, the biochemist Rosalind Yalow, reminded us through her work about measurable biomarkers: what circulates in the blood reveals much about risk and resilience. Today, it is evident: not only fats regulate cholesterol. High-fiber snacks work silently yet effectively. Those seeking high performance and longevity can steer their lipid profile in the right direction with small, smart bites.
Cholesterol is a vital lipid, a building block for cell membranes and hormones. It becomes problematic when LDLLow-Density Lipoprotein; transports cholesterol into tissues, associated with atherosclerosis when elevated is persistently high, while HDLHigh-Density Lipoprotein; returns excess cholesterol to the liver tends to have a protective effect. Fiber consists of indigestible carbohydrates. Particularly relevant are soluble fibersbind bile acids in the intestine, promote excretion, thereby reducing cholesterol synthesis in the liver, such as those from legumes, nuts, whole grain rye, or psyllium husks. They slow down gastric emptying, modulate glucose and insulin responses, and nourish the microbiomegut ecosystem of microorganisms; produces short-chain fatty acids that influence liver metabolism. For performers, this means stable energy, reduced inflammation, better vascular health – and thus more cognitive and physical performance reserves.
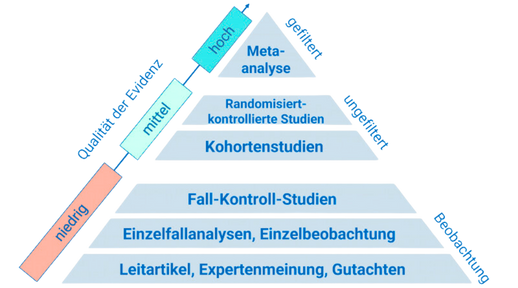
A daily cup of beans can significantly lower LDL cholesterol: in a randomized, controlled crossover study, 1 cup (approx. 180 g) of mixed canned beans over four weeks reduced total and LDL cholesterol compared to white rice, while a half serving did not reliably reproduce the effect [1]. Animal data on mung beans additionally suggest reduced liver fat and less inflammatory liver tissue – more pronounced after germination [2]. While nuts provide fat, they improve the lipid profile: a meta-analysis of 113 RCTs showed moderate reductions in total and LDL cholesterol as well as small benefits in triglycerides and ApoB, without affecting HDL [3]. Whole grain rye compared to refined wheat can increase HDL and reduce liver fat – evidence of better lipid modulation despite unchanged glycemia in an animal model [4]. Psyllium husks, a concentrated source of soluble fiber, lowered total and LDL cholesterol in a three-week observational study of hypercholesterolemia; gastrointestinal complaints were usually transient [5]. The essence: fiber-rich snacks adjust the lipid profile in a cardioprotective direction – with side effects that are rather positive: satiety, better blood sugar curves, and a more active microbiome.
The strongest evidence for legumes comes from randomized dietary changes in everyday life: in a multicenter, randomized crossover study, participants changed their daily side dish for four weeks. A serving of 1 cup of beans lowered LDL by about eight percent compared to a white rice control phase; half servings showed no robust advantage. Practically relevant: using canned instead of preparing from scratch worked just as well – making adherence likely [1]. Concurrently, preclinical data illustrate why legumes are liver-friendly: in a hamster model on a cholesterol-rich diet, cooked and germinated mung beans reduced total and non-HDL cholesterol, increased cholesterol excretion with stool, and dampened liver fat accumulation and inflammation – with additional benefits from germination [2]. For nuts, a large meta-analysis of 113 RCTs provides robust estimates: about 45 g of nuts daily consistently lowered total and LDL cholesterol and improved atherogenic ratios, without significantly altering HDL – a strong signal across various populations [3]. Additionally, a controlled animal model shows that unfermented whole grain rye increases HDL and reduces liver lipids compared to refined wheat – indicating the special role of whole grain fibers and their fermentation products in the gut [4]. Finally, a prospective observational study on psyllium husk supplementation demonstrates that just three weeks are sufficient to noticeably lower LDL, with initial digestive discomfort usually subsiding – a realistic, low-threshold tool for everyday use [5].
- Consume 1 cup (approx. 180 g) of legumes daily: rinse canned beans and add to a bowl or soup. The 1-cup sweet spot showed significant reductions in total and LDL cholesterol compared to white rice in an RCT [1]. Keep it varied: lentil dal, chickpea salad, black beans in chili. Animal data on mung beans suggest additional liver benefits – even stronger when germinated [2].
- Incorporate 30–50 g of raw or lightly roasted nuts as a snack: replace afternoon pastries with almonds, walnuts, or hazelnuts. The meta-analysis of 113 RCTs shows consistent reductions in total and LDL cholesterol and better atherogenic ratios [3]. Tip: unsweetened, unsalted; use as a crunch over yogurt or salad.
- Replace white flour: opt for whole grain rye sandwiches or wraps. Compared to refined wheat, whole grain rye showed more favorable lipid modulation in a controlled model, including higher HDL and less liver fat [4]. Practice: rye bread with hummus and vegetables; whole grain wrap with beans, avocado, leafy greens.
- Mix 1–2 teaspoons of psyllium husks into yogurt or smoothies daily: start low (1 tsp) and drink an additional glass of water, increasing as tolerated. A prospective study showed declining total and LDL values within three weeks; initial digestive symptoms usually diminish [5].
Fiber-rich snacks are more than side dishes – they are precise tools for a better lipid profile and thus for longevity and performance. In the coming years, personalized fiber plans tailored to microbiome signatures are likely to further optimize LDL reduction. Those who start today are building the metabolic foundation on which future precision medicine can maximally operate.
This health article was created with AI support and is intended to help people access current scientific health knowledge. It contributes to the democratization of science – however, it does not replace professional medical advice and may present individual details in a simplified or slightly inaccurate manner due to AI-generated content. HEARTPORT and its affiliates assume no liability for the accuracy, completeness, or applicability of the information provided.