The common misconception: drug use primarily stems from "poor discipline." The data paint a different picture. Stress – whether from job pressure, social isolation, or ongoing internal tension – shifts the reward system and increases vulnerability to substances. Surprisingly, even targeted physical activity can reduce cravings and the risk of relapse, while too much caffeine can even exacerbate stress [1] [2].
Stress is more than just a feeling. It activates the hypothalamic-pituitary-adrenal axishormonal stress regulation system, raises cortisol levels, and modulates the reward systemneural circuits for motivation and pleasure, e.g., VTA–nucleus accumbens. Under persistent strain, the brain reacts more strongly to immediate rewards as cognitive control diminishes – creating a perfect breeding ground for “quick fixes” like substance use. Simultaneously, homeostasisinternal balance is disrupted, affecting sleep, appetite, and mood. Crucially, stress is modifiable. Strategies that integrate body (exercise), mind (mindfulness), relationships (social contacts), and professional support address the biological and psychological drivers simultaneously.
Chronic stress increases vulnerability to substance use and complicates abstinence. Studies show that lack of family support correlates with increased depression, PTSD symptoms, and greater substance use severity – social friction thus amplifies stress and addiction pathways [3]. Conversely, structured exercise programs can moderately reduce stress and depressive symptoms and enhance quality of life – a relevant lever for relapse prevention [1]. Everyday “coping tricks” can also be harmful: high caffeine intake correlates with significantly heightened stress levels; those who "treat" stress with coffee often pay with increased inner turmoil [2]. Mindfulness-based interventions have been shown to reduce perceived stress and substance cravings – particularly valuable in vulnerable groups [4].
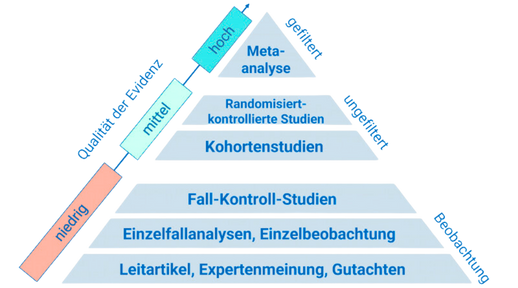
Two lines of evidence are particularly applicable. First: exercise as a therapeutic component in substance use disorders. Systematic evaluations of randomized controlled trials show that physical activity reduces stress and depressive symptoms and enhances quality of life; there are indications of reduced craving, although further precision research is needed [1]. Reviews emphasize that exercise can be integrated into treatment programs when motivation and adherence are deliberately supported – for example, through goal setting, experiential learning, and motivational interviewing [5]. Second: mindfulness as a stress dampener. In clinical pilot studies with opioid-dependent individuals, brief MBSR programs significantly reduced perceived stress, emotional regulation problems, and substance cravings – an indication that even low-threshold, structured practice positively influences neuropsychological stress and craving processes [4]. Additionally, a randomized group therapy study in AUD with co-use found that Mindfulness-Oriented Recovery Enhancement reduced cravings more than a supportive control across stress- and cue-loaded protocols – a signal for transferable effects in polysubstance use [6]. The social dimension acts as a biological amplifier: evidence regarding isolation and loneliness describes HPA-axis dysregulation, glucocorticoid resistance, and pro-inflammatory patterns that enhance anhedonia and withdrawal – mechanisms that can promote addictive behavior [7]. Meanwhile, longitudinal data indicate that family conflicts and low support predict more severe courses, while peer support fosters early improvements [3].
- Integrate 150–300 minutes of endurance training per week plus 2 strength sessions. Start small: 10 minutes of brisk walking after stressful meetings, then progressively increase. Exercise lowers stress and depressive symptoms and supports abstinence strategies [1] [5].
- Practice mindfulness daily for 10 minutes: breath focus (4–6 breaths/minute) or body scan. Use a 6-week structure: one weekly guided session plus brief daily practice. Goal: expand the stimulus-response gap, let cravings pass [4].
- Seek professional help: inquire about programs with Mindfulness-Oriented Recovery Enhancement or CBT elements. These approaches reduce cravings even under stress triggers and are promising for polysubstance use [6].
- Strengthen your support network: plan two regular social contacts per week (family, friends, support group). Reduce sources of conflict early, increase peer support – this measurably improves outcomes [3].
- Curb stress-related caffeine: limit caffeine to <200–300 mg/day and avoid late doses. High consumption is associated with increased stress levels – especially during high-pressure phases [2].
Stress is not a character test but a neurobiological state – and it is deliberately changeable. Move wisely, practice mindfulness, build your network, and seek support when stress drives consumption. Start today with 10 minutes of movement and 5 minutes of breath focus – the curve of your health begins now.
This health article was created with AI support and is intended to help people access current scientific health knowledge. It contributes to the democratization of science – however, it does not replace professional medical advice and may present individual details in a simplified or slightly inaccurate manner due to AI-generated content. HEARTPORT and its affiliates assume no liability for the accuracy, completeness, or applicability of the information provided.