The neuroscientist and former director of the US National Institute on Drug Abuse, Nora Volkow, has coined an insight that has transformed the field: addiction is not a moral weakness, but a treatable brain disorder. This shift in perspective opens the door for empathy – and for strategies that work. Those who want to live high performance need not only self-leadership but also social intelligence: actively supporting people in their environment in their recovery. This is good for them – and promotes resilience, meaning, and connection in one’s own life.
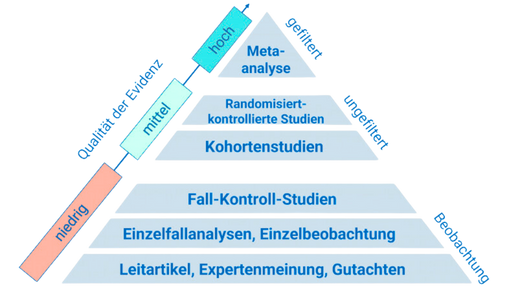
Substance use disorder SUDpattern of problematic consumption with loss of control, distress, and functional impairments arises from an interplay of genetics, environment, stress, and neurobiological adaptations. Core symptoms are craving Cravingintense desire for the substance, reduced self-control, and increased stress reactivity. Social support soziale Unterstützungreliable emotional, informational, and practical assistance from others is one of the strongest protective factors – it intercepts relapses, strengthens motivation, and builds sustainable routines. Mindfulness Mindfulnessnon-judgmental awareness of the moment and cognitive strategies Copingconcrete thinking and behavior strategies for reducing stress and triggers enhance control in high-risk situations. Digital tools Digital Healthapps and platforms for support, communication, and self-monitoring can structure and make these processes visible.
Activating social networks not only reduces consumption spikes but also improves mood, physical stability, and the sense of belonging. In embedded peer programs, participants reported reductions in substance use or abstinence as well as better mental and physical health and stronger connections [1]. Web-based communities provide low-threshold informational and emotional support – especially in early phases, where affected individuals often seek factual guidance [2]. Mindfulness training addresses the hyperactivity of the stress system and strengthens prefrontal control networks; in studies, craving decreases and – among smokers – even consumption drops significantly [3] [4]. Failure to involve family, on the other hand, misses potential: although professional teams recognize the benefits, it is still too rarely utilized systematically – a shortcoming that measurably weakens engagement and outcomes [5]. Digital companions enhance treatment adherence, particularly in medication-assisted programs, by consolidating monitoring, messaging, and resources; early active use correlates with better 30-day retention [6].
Several research threads coalesce into a clear picture. First: socially-supported recovery. A mixed-methods pilot study integrating SMART Recovery into outpatient programs showed widespread acceptance and various benefits beyond standard care – less consumption, better mental and physical health, and stronger social connections. The switch to online formats during the pandemic maintained the benefits, emphasizing the flexibility of the approach [1]. Complementarily, an analysis of the Reddit community r/OpiatesRecovery over eight years shows that self-disclosure strategically attracts different forms of support: information-seeking openness leads to more concrete advice, while emotional openness draws empathetic responses and shared experiences. Early stages of addiction receive a lot of advice but less emotional support – a signal for moderators and peer coaches on where to focus [2]. Second: training for more self-control. Randomized studies on mindfulness show that even brief interventions increase activity in the anterior cingulate cortex and medial prefrontal cortex – regions responsible for emotional and impulse control. Among smokers, this reduced stress and in one study decreased consumption by around 60% after two weeks, compared to no effect in the relaxation control group [3] [4]. A review contextualizes: acute cravings can be reduced through cognitive overload, while repeated practice may diminish the stimulus-response coupling long-term – mindfulness is not the only, but a particularly practical strategy [7]. Third: structure beats intention. A large-scale implementation project tested an app for supporting OUD patients in 53 clinics. High acceptance, early app interaction, and proactive messaging from professionals were associated with a significantly improved 30-day treatment retention compared to historical data [6]. Lastly, behavioral psychological programs based on the TPB show that targeted training of knowledge, attitudes, norms, and self-efficacy reduces relapses over time; cognitive-behavioral interventions, also led by nursing professionals, reduce craving and strengthen coping in prison contexts – even with limited resources [8] [9].
- Build real and digital support networks: Search for or establish a SMART or similar peer group and link it with an online forum (e.g., moderated communities). Aim: to participate weekly, document goals in writing, and reflect progress in a buddy system. Studies show additional effects beyond standard treatment and meaningful online interactions [1] [2]. Supplement this with curated recovery feeds or closed groups, as many affected individuals effectively use social media – especially younger people and women [10].
- Integrate mindfulness as a craving intervention: Practice a focused breathing or body scan sequence for 10–15 minutes daily and a 3-minute "STOP" micro-pause (Stop – Breathe – Observe – Proceed), especially when facing triggers. Short formats reduce stress and enhance prefrontal control; among smokers, consumption significantly decreased in studies [3] [4]. Repetition consolidates the effect and interrupts stimulus-response patterns [7].
- Develop a personal relapse prevention plan: Identify high-risk situations, formulate If-Then plans ("If I feel X, then I will call Y and walk briskly for 10 minutes"), and practice cognitive restructuring ("Craving is a wave, not a command"). TPB-based programs reduced relapses; CBT modules decreased craving by about one-third and significantly strengthened coping domains [8] [9].
- Use digital helpers consistently: Choose a recovery app with self-monitoring, secure messaging, and a resource library. Arrange check-ins with the treatment team in the first 30 days – early, bidirectional interaction increases commitment to therapy [6]. Activate notifications for trigger days and link the app with a calendar for appointments to groups or sports.
- Involve family and close loved ones: Invite a trusted person to an informative discussion and goal-setting session; define clear support roles (e.g., transportation to meetings, shared evening routines). Many teams still underutilize family members – your proactive step can close the gap and stabilize recovery [5].
The future of addiction treatment is connected, personalized, and practical: peer communities, neuroplastic training through mindfulness, and digital companions interlink. Smarter apps with adaptive coaching and systematic family involvement are to be expected – enabling empathy to have measurable impact and recovery to become a high-performance competence.
This health article was created with AI support and is intended to help people access current scientific health knowledge. It contributes to the democratization of science – however, it does not replace professional medical advice and may present individual details in a simplified or slightly inaccurate manner due to AI-generated content. HEARTPORT and its affiliates assume no liability for the accuracy, completeness, or applicability of the information provided.