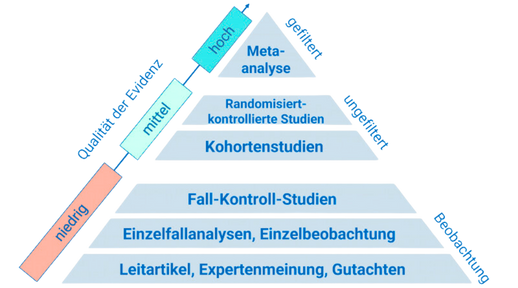
As a cardiologist and scientist, Elizabeth Blackburn, Nobel laureate for her work on telomeres, has demonstrated how psychological stress can accelerate biological aging processes down to the cellular level. This perspective changes the way we think about heart health: it's not just cholesterol, exercise, and nutrition that count, but also our internal stress levels. For high performers, this means that those who manage stress wisely not only protect their performance but also their heart—measurably, trainably, daily.
Stress is a physiological alarm response regulated by the autonomous nervous systemsubconscious control center for heart, blood pressure, breathing, especially by the sympathetic nervous system, and the HPA axishormonal stress axis consisting of the hypothalamus, pituitary gland, and adrenal cortex. In the short term, it helps mobilize performance. However, chronic stress keeps pulse and blood pressure elevated, promotes inflammation, and disrupts vascular function. Crucial for the heart is heart rate variability (HRV)fluctuation between heartbeats; high HRV = flexible stress regulation, a marker for the balance between the sympathetic and parasympathetic nervous systems. Equally relevant is visceral fatadipose tissue around the internal organs, which is favored by stress hormones and releases inflammatory mediators. Sleep acts as a nightly "reset" for blood pressure and the stress system—if it fails, homeostasis tips.
Unregulated stress increases blood pressure and heart rate, decreases HRV, and thus drives cardiovascular risks higher. Systematic reviews demonstrate that targeted relaxation techniques such as progressive muscle relaxation and breathing exercises reduce blood pressure, anxiety, and stress in heart patients while improving quality of life—with positive effects on pulse and blood pressure regulation [1]. Mindfulness and yoga interventions improve HRV and concentration, showing indications of enhanced emotional regulation and physiological "parasympathetic tone"—a protective signal for the heart [2] [3]. Conversely, stress-induced sleep deprivation exacerbates hypertension, arrhythmias, and coronary risks; in particular, sleep apnea increases sympathetic activation, inflammation, and endothelial damage—a clear pathway to arrhythmias and cardiovascular events [4].
A recent systematic review of relaxation techniques in cardiovascular populations consistently shows: progressive muscle relaxation, breathing training, and biofeedback reduce blood pressure and stress symptoms and enhance well-being. Relevance for practice: these methods simultaneously address physiological and psychological components and can be integrated into rehabilitation and daily programs [1]. In a randomized study with healthy individuals, eight weeks of mindfulness-based exercises or yoga led to improvements: yoga shifted HRV toward higher parasympathetic activity, while mindfulness increased mindfulness ability and concentration—both building blocks of a robust stress response and thus potentially cardioprotective [2]. Additionally, an observational study among clinical staff showed that individual mindfulness exercises such as body scan, deep breathing, and grounding acutely improved HRV and reduced subjective stress—a suggestion that brief, practical interventions can trigger measurable physiological relaxation [3]. Finally, a three-armed, randomized smartphone trial provides early evidence that app-based stress management with integrated HR biofeedback can reduce perceived stress more effectively than a waitlist; both active variants improved emotional regulation and well-being. The authors emphasize the importance of personalized, sensor-based approaches for greater efficacy and sustainable engagement [5].
- Breath as a lever: Practice diaphragmatic breathing for 5–10 minutes (4 seconds in, 6 seconds out) or progressive muscle relaxation. Goal: noticeably calmer pulse, warmer hands—signs of the parasympathetic nervous system. Studies show blood pressure reduction and less stress in heart patients [1].
- Mindfulness in microdoses: Start your day with 8 minutes of body scan or 10 slow breaths plus a brief body scan sequence in the evening. HRV improvements and less subjective stress have been observed after individual sessions [3]. Over 8 weeks, mindfulness trains concentration and stress regulation, while yoga enhances HRV [2].
- Focus blocks for protection: Plan 90-minute deep work sessions without interruptions, followed by 10 minutes of breathing or walking meditation. Regularity trains the stress system. Mindfulness can favorably influence HPA and SNS markers in the long term—potentially cardioprotective [6].
- Sleep as heart protection: Establish a "digital twilight" 60 minutes before sleep and use 6–8 slow breathing cycles to fall asleep. This stabilizes the nightly blood pressure drop and reduces sympathetic overactivity. Otherwise, sleep deprivation increases the risk of hypertension and arrhythmias [4].
- Smart time management: Use a smartphone-based stress and focus plan (e.g., appointments with breathing prompts, brief mood check-ins, optional HR feedback). An 18-day app program with HR-based biofeedback reduced perceived stress more than no intervention; both active variants improved emotional regulation and well-being [5].
The next wave is personalized: apps with real-time HRV, AI-driven recommendations, and context-sensitive prompts could tailor mindfulness, breathing, and time management precisely to your stress profile [5]. Future studies should clarify the duration, dosage, and combinations of breathing, mindfulness, and sleep interventions—with hard cardiovascular endpoints and practicality in view [1] [2].
This health article was created with AI support and is intended to help people access current scientific health knowledge. It contributes to the democratization of science – however, it does not replace professional medical advice and may present individual details in a simplified or slightly inaccurate manner due to AI-generated content. HEARTPORT and its affiliates assume no liability for the accuracy, completeness, or applicability of the information provided.