Imagine a future where cardiovascular diseases in women are significantly less common – not through expensive high-tech interventions but through precise nutrition and a smart micronutrient strategy. In this vision, magnesium is a silent game changer: an unassuming mineral that stabilizes blood pressure, rhythm, and vascular health – thus protecting performance for decades. This future begins today, with every meal and every conscious decision.
Magnesium is an essential mineral involved in over 300 enzymatic reactions – from energy metabolism to the electrical stability of the heart. It modulates endothelial functionthe performance of the inner vascular layer that regulates blood flow and vascular tone and ionic homeostasisbalance of mineral ions such as calcium and potassium that control heart rhythm and muscle contraction. Particularly relevant: women, especially during and after menopause, experience hormonal and metabolic changes that burden vascular health. It is precisely here that magnesium acts as a "molecular buffer" against inflammation, oxidative stress, and arrhythmias [1] [2]. Those who predominantly consume a Western diet often have lower magnesium intake than recommended – especially when whole grains, legumes, and green leafy vegetables are rarely on their plates [2].
Low magnesium status consistently correlates with a higher risk of hypertension, coronary calcification, stroke, atrial fibrillation, heart failure, and cardiac mortality [2]. In a large cohort of postmenopausal women, low magnesium intake was associated with an increased risk of hospitalization for heart failure – particularly for the form with reduced ejection fraction, which weakens the heart's pumping power [3]. Clinically, magnesium deficiency often presents insidiously: muscle cramps, fatigue, or palpitations may be precursors; in the case of pronounced deficiency, arrhythmias may arise that can rapidly improve after magnesium administration [4] [5]. Magnesium also matters indirectly: thiazide or loop diuretics increase the loss of magnesium and potassium – resulting in a higher risk of arrhythmias after myocardial infarction; magnesium-sparing strategies reduce ectopic beats and stabilize rhythm [6].
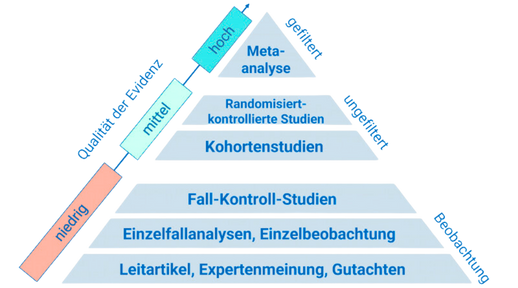
Three lines of evidence paint a clear picture. First: population data. Analyses from the past two decades link low intake or serum magnesium to a broad range of cardiovascular risks – from hypertension to heart failure. These associations are supported by metabolic studies showing that even mild deficiencies trigger inflammation and oxidation processes, dyslipidemia, and endothelial dysfunction – mechanisms that respond positively to magnesium [2]. Second: women's health. In the WHI cohort, the risk of heart failure in postmenopausal women significantly increased in the lowest magnesium quartile compared to the highest; notably, there was a stronger association with systolic pumping weakness, indicating a role for magnesium in myocardial excitation-contraction coupling [3]. Third: dietary quality. A high score of magnesium-rich foods – including whole grains, nuts, vegetables, legumes, coffee, and tea – was associated over three decades with a lower risk of cardiovascular events and coronary artery disease, facilitating the real-world application of the evidence [7]. Additionally, intervention data show that polyphenol-rich dark chocolate improves endothelial function (measured as flow-mediated dilation) and can positively influence inflammation and platelet activity – effects that are cardiovascularly relevant and also provide magnesium [8] [9].
- Consider a magnesium supplement if your diet has gaps: typically 200–400 mg of elemental magnesium per day, preferably in well-tolerated forms such as citrate, glycinate, or malate; consult your doctor beforehand, especially if you have kidney insufficiency or are taking medications [2] [1].
- Commit to including whole grains: swap white bread for 100% whole grain, choose oats, barley, or brown rice – aim for 2–3 servings per day. This lowers cardiovascular risk and sustainably increases magnesium intake [10] [2] [7].
- Use dark chocolate strategically: 1–2 small pieces (≥70–80% cocoa) after meals. This way, you combine magnesium with flavonoids that are proven to improve endothelial function, positively influence lipids, and dampen platelet activity [8] [9].
For high performers, magnesium is an underestimated lever for heart protection, energy, and long-term performance. Next steps: check your daily intake from whole grains, legumes, and green vegetables, incorporate moderate amounts of dark chocolate – and clarify the appropriate supplementation dose medically if needed.
This health article was created with AI support and is intended to help people access current scientific health knowledge. It contributes to the democratization of science – however, it does not replace professional medical advice and may present individual details in a simplified or slightly inaccurate manner due to AI-generated content. HEARTPORT and its affiliates assume no liability for the accuracy, completeness, or applicability of the information provided.