Imagine a future where your personal health stack not only includes wearables and blood values, but also a precisely cultivated ecosystem of microbes. Parents are already storing umbilical cord blood today—why not tomorrow also the child's "microbiome profile" as immunological capital? This vision is closer than we think. The microbes in our gut are not bystanders; they are co-engineers of our defense. Those who nurture them gain resilience, energy, and longevity.
The gut flora—correctly referred to as the microbiometotality of microorganisms in and on our body—is in constant communication with the immune systemnetwork of cells, tissues, and signals that defend against pathogens and facilitate tissue repair. Particularly critical is the gut barriermucus layer, epithelial cells, and immune boundary that allows nutrients through while keeping pathogens out. Microbes produce metabolitesmetabolic products such as short-chain fatty acids that train immune cells and seal the barrier. When this ecosystem is thrown off balance—a dysbiosisloss of diversity and functional balance of the gut microbiota—the propensity for inflammation increases. For high performers, this means: less recovery, greater susceptibility to infections, and poorer metabolic regulation. The good news: Nutrition, exercise, and stress management can measurably alter the microbiome within weeks—and thus improve your immune performance.
A modern, one-sided dietary profile rich in sugar and ultra-processed foods reduces microbial diversity, weakens the barrier, and promotes chronic inflammation—a risk profile for obesity, diabetes, and immune-driven diseases [1]. Experiments show that added sugar can displace protective gut bacteria; thus, Th17 immunity decreases, fat absorption increases, and metabolic disorders rise—a clear link between sugar spikes, microbiome shifts, and immunodeficiency [2]. Antibiotics are life-saving but disrupt the microbiome: from reduced species diversity to fewer short-chain fatty acids and barrier loss—consequences that can promote infection risks and inflammation [3]. Not only pills make the difference: Chronic stress alters the gut community and promotes systemic and neural inflammation through the microbiota-gut-immune-brain axis—resulting in mental and immunological consequences [4]. In contrast, regular physical activity expands microbial diversity and strengthens immunometabolic resilience, boosting both performance and defense [5][6].
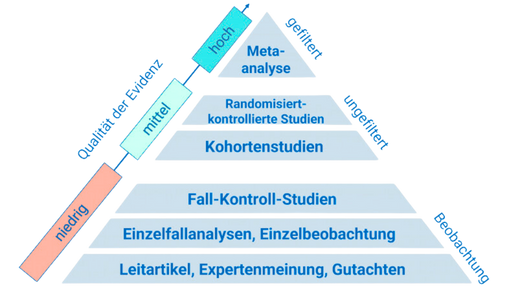
The role of diet as a microbiome driver is well established: A recent overview shows that modern, fiber-poor, sugary, and fatty diets decimate the biodiversity of gut microbes, reduce the production of protective metabolites, increase gut permeability, and thus fuel chronic inflammation, obesity, and metabolic diseases. Conversely, diversified, fiber-rich diets with unsaturated fats and plant protein promote a robust, diverse microbiota, strengthen the barrier, and enhance the synthesis of protective compounds—resulting in a direct benefit for immunity [1]. Mechanistically, an experimental study specifies the sugar effect: In an animal model, added sugar replaced beneficial bacteria with pathobiont species, dampened Th17-mediated protective mechanisms, and increased fat absorption and weight gain—a plausible pathway from sweetness to immune and metabolic stress [2]. A third element concerns antibiotics: A comparison of commonly prescribed agents shows massive differences in microbiome disruption. Clindamycin caused a lasting dysbiosis with significantly reduced short-chain fatty acids and a damaged mucus barrier, while azithromycin had milder, reversible effects. These differences are clinically relevant when therapeutic alternatives exist and microbiome protection is a priority [7].
- Integrate fermented foods daily: Natural yogurt, kefir, sauerkraut, or kimchi provide live cultures that can modulate mucosal immunity and barrier function. Start with 1 serving per day and gradually increase as tolerated [8].
- Reduce free sugar: Keep added sugar below 25–30 g/day. Swap sweet snacks for fruit plus nuts and choose drinks without added sugar. This protects Th17-dependent defense mechanisms and prevents microbial shifts [2].
- Eat for diversity: "30 plants per week" as a simple metric. Beans, whole grains, vegetables, herbs, nuts, and olive oil provide fibers and polyphenols that make the microbiota more diverse and immune stronger [1].
- Use antibiotics wisely: Only weigh options with clear indications and drug choices. When alternatives exist, prefer substances with lower microbiome effects; note that some agents (e.g., clindamycin) can promote long-term dysbiosis [7]. Discuss a "microbiome-sensitive" therapy with your doctor.
Your microbiome is a trainable ally. Feed it wisely, protect it from unnecessary disruptions, and it will strengthen your immunity—noticeable in energy, resilience, and performance. Start this week: one serving of fermented foods daily, halve your sugar intake, increase plant diversity, and use antibiotics mindfully.
This health article was created with AI support and is intended to help people access current scientific health knowledge. It contributes to the democratization of science – however, it does not replace professional medical advice and may present individual details in a simplified or slightly inaccurate manner due to AI-generated content. HEARTPORT and its affiliates assume no liability for the accuracy, completeness, or applicability of the information provided.