The widespread myth: “I can immediately tell when something is wrong – I don’t need screening.” The reality is both sobering and hopeful: Many breast tumors are neither palpable nor painful in the early stages, but are highly treatable with modern early detection. At the same time, new data shows that informed self-measures – from smart self-examination to risk adaptation through genetics – can bridge the gap between chance and prevention [1] [2].
Breast cancer develops when cells in the breast tissue grow uncontrollably and bypass the body’s own control mechanisms. Early detection is crucial before metastases occur. Early detection includes structured programs (e.g., mammography) and individual measures. Breast self-examination BSEregular, systematic palpation of the breast and armpit increases awareness of changes. Risk factors are partially modifiable: overweightexcessive body fat mass, often associated with chronic inflammation and hormonal imbalances particularly increases the risk after menopause. Diet and exercise influence central metabolic pathways (insulin, inflammation). Additionally, there are hereditary components: predictive genetic teststesting for mutations that increase lifetime risk to personalize prevention and monitoring help identify high-risk individuals [2]. For high performers, early detection is a performance tool – it preserves health spans, prevents therapy failures, and maintains energy and joy of life.
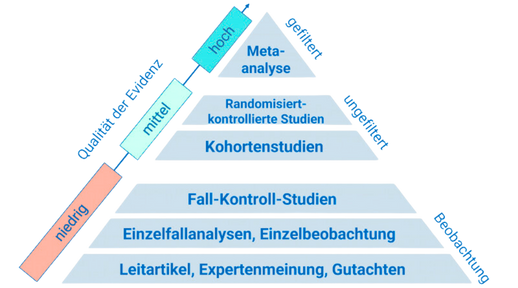
Health effects begin with risk reduction: A healthy body weight and regular activity lower cancer risk through several pathways – including reduced chronic inflammation and more favorable hormone profiles; European recommendations emphasize movement, weight management, and limiting sedentary behavior [3]. Conversely, obesity is linked to unfavorable biology, later diagnosis, and worse outcomes; the cascade of insulin resistance, pro-inflammatory cytokines, and altered adipokine signatures promotes tumor growth and therapy resistance [4] [5]. On the behavioral level, structured education on BSE shows a significant increase in competence and implementation rates – women examine themselves more frequently and with greater confidence, reporting improved quality of life [1]. Those with a hereditary high risk can initiate targeted prevention and monitoring strategies through predictive testing, which may reduce morbidity and mortality [2].
A European review on cancer prevention highlights that diet, body weight, physical activity, sitting, and breastfeeding substantially influence the cancer burden. Specifically, the ECAC5 recommends a plant-based diet rich in whole grains, vegetables, legumes, and fruits, as well as avoiding overweight and prolonged sitting – measures that lower the risk for several types of cancer and support breast health [3]. A systematic review on diet and breast cancer confirms the preventive value of plant-rich patterns like the Mediterranean diet; moreover, data suggest that dietary strategies may also favorably influence relapse risks for survivors – a clear argument for integrating nutrition into oncological practice [6]. On the risk stratification side, literature on predictive genetic testing shows that identifying hereditary mutations enables personalized prevention (intensive screening, chemoprevention, or prophylactic options) and thus reduces mortality – despite ethical and organizational challenges [2]. Together, these findings create a framework: lifestyle measures lower baseline risk, while genetic information precisely addresses high-risk groups – a dual safety line for longevity and performance.
- Make breast self-examination a routine: Once a month, a few days after the period, systematically palpate in the mirror, standing and lying down; note any abnormalities and seek medical advice if uncertain [1].
- Stabilize your body weight within a healthy range: Combine daily physical activity (e.g., 8,000–10,000 steps) with 150–300 minutes of moderate endurance exercise plus 2 strength sessions per week; actively reduce sitting times (Pomodoro breaks) [3].
- Eat a plant-based and colorful diet: Fill every meal with vegetables/fruits, add whole grains and legumes, limit red meat, and avoid processed meat; this supports a favorable inflammatory and hormone profile [3] [6].
- Check your individual risk: If there is a family history or early diseases in the family, talk to your doctor about predictive genetic tests and – if at high risk – about intensive screening or prophylactic medications as options [2].
The future of breast cancer early detection is hybrid: precise genetics, intelligent imaging, and behavior-based prevention interconnect. We can expect new tools – from AI-supported risk prediction to personalized nutrition programs – that make early detection even earlier and prevention even more effective.
This health article was created with AI support and is intended to help people access current scientific health knowledge. It contributes to the democratization of science – however, it does not replace professional medical advice and may present individual details in a simplified or slightly inaccurate manner due to AI-generated content. HEARTPORT and its affiliates assume no liability for the accuracy, completeness, or applicability of the information provided.